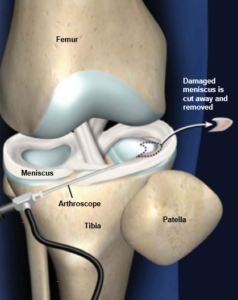
Over the last thirty years the advances in musculoskeletal imaging and surgical arthroscopy have increased the surgical options and minimized the post-operative morbidity from tears of the knee meniscus. Generally, there is a mild effusion, minimal pain, and a rapid recovery of range of motion when part, or even all, of a meniscus is removed. Also, very often the ability to perform basic activities of daily living returns in a relatively short period of time. Certain studies represented by Goodwin et al (1), demonstrate no difference in recovery between patients undergoing rehabilitation and those recovering without such assistance during the early recovery phase. The need for formal rehabilitation and post-op training appears to be less warranted, but there is much evidence that this is a misconception.
Problems with Research
One problem in basing decisions on this research is that the comparisons are soon after surgery, and the outcome measures are not directly related to functional performance. There have been a number of studies that report strength deficits many months (2) and years (3) after surgery. Even though strength is often measured on non-functional testing equipment, the deficits are likely to affect performance. Ericcson et al (3) included more functional measures of single leg rising from a flexed position and single leg squats and found deficits even 4 years after surgery.

Individual Successes

Not all post-operative patients will need a formal functional training program, but many would benefit greatly. Certain studies represented by Haviv et al (4) have attempted to identify certain demographic groups that are more likely to have a less positive result. But even these predictors are averages. In order to provide each individual with the optimum post-operative care, functional testing movements must be utilized to determine each individual’s specific movement success. Functional movements that engage the entire body in all three planes of motion can quickly indicate where deficits in motion (mobility) and control of motion (stability) exist. Often these global movements are combined with more localized, but still integrated, test movements in order to identify specific impairments.
The Joint Caught in the Middle

Dr. Gary Gray has described the knee as the joint caught in the middle (between the foot and the hip), with few places to go (to protect itself) and nowhere to hide (from the forces transmitted through the foot and hip). Here at Superior Physical Therapy an important maxim is “the test is the exercise and the exercises are the test”. From a practical point of view, this means that a functional movement test that identifies a deficit can (and should) be tweaked to create an exercise movement that can begin to “fix” the problem.
Logic also tells us that the knee is susceptible to injury when the foot and hip have asymptomatic limitations or impairments. Superior Physical Therapy provides logical strategies based on the principles of human movement that can turn the “perpetrators” of the injury, symptoms, or residual dysfunction into the “purveyors” of health and resumption of desired activities.
The strategies for creating more motion and control of motion at the hip and foot should integrate the knee into the functional movements. Using the Chain Reaction principle, both top-down drivers to address the hip and bottom up drivers to work on the foot can be implemented early after surgery to eliminate deficits or enhance function while still keeping the knee integrated with the rest of the body. Once the hip and foot are functioning well (“perpetrators” eliminated), then movements that increase the demands on the knee can begin. Again, these movements/exercises must be integrated. This allows the “causative cures” phenomenon to be manifested. The joints (hip and foot) that may have been the cause are transformed into powerful protectors of the knee, reducing symptoms and enhancing function.
If the goal of knee surgery is to have a patient who is more functional, has less pain, and is overall a happy patient then It would be wise to address the underlying cause of the meniscus tear, especially for non-contact injuries. There is overwhelming evidence that doing nothing after a meniscectomy will result in a patient who is less functional and has a higher risk for reinjury of the knee. If you want to ensure that your patient has an improved quality of life after surgery send them to Superior Physical Therapy for a full body assessment in order to address the underlying cause of the tear, which is most likely due to a dysfunction in either the foot or the hips, not the knee.



